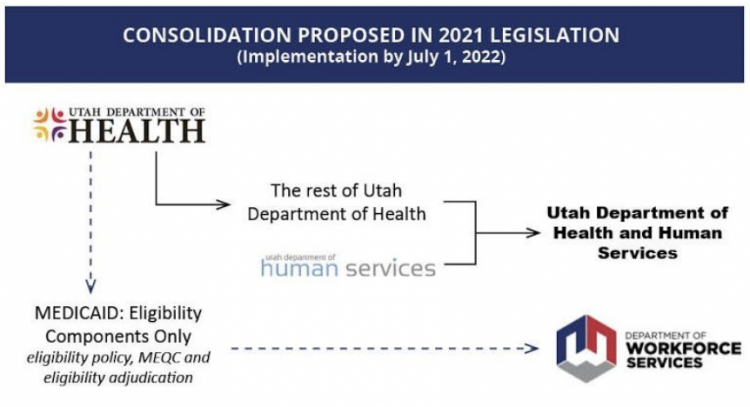
Utah cannot afford a delay in improving delivery of critical services to our underserved and marginalized communities. To ensure we have the right structure in place that better serves individuals and families as quickly as possible, the Executive Office of the Governor, working with Rep. Paul Ray, supports passage of a bill during the 2021 general legislative session that would authorize the merger of the state’s two primary social service agencies: the Utah Department of Health (UDOH) and Department of Human Services (DHS), creating the Utah Department of Health and Human Services.
The bill would also move Medicaid eligibility components from the Department of Health to the Department of Workforce Services (DWS). These functions include Medicaid eligibility policy, Quality Control (MEQC), and eligibility adjudications. The proposed change would not move all of Medicaid to Workforce Services, only the economic eligibility components.
Please share your feedback, especially in the following three areas:
- Resources: Considerations on personnel and financial resources to complete the merger
- Staged Approach/Planning: Considerations on avoiding impacts on individual and family stability, efficient delivery of quality services, communities of color, and private providers and partnerships
- Cost-benefit analysis
- Metrics to track customer experience, outcomes, efficiencies
- Legal: Updates needed to code, policies, contracts and agreements; effects to local, state and federal compliance
Send written comments to: [email protected].
Frequently Asked Questions
You can download these FAQ’s here.
What challenges exist in the current structure that could be addressed by a consolidation of agencies?
There is an opportunity for us, as a government, to think differently about how we serve the public. We work collaboratively now, but we’re not necessarily designing programs together. There can be boundaries between agencies that are hard to cross, and having multiple systems doing similar tasks complicates things. Bringing the agencies together would allow for improvements in coordination and, ultimately, a better delivery of services and outcomes.
How do we envision stakeholder and public input shaping the agency consolidation?
We look forward to a robust process, including stakeholder and public input, as we make decisions on how best to consolidate agencies. During drafting, and if and when a bill is passed, we want to hear from you. We invite feedback and communication to create a successful final product.
There will be technical aspects that are part of the process as we move forward and there will be regular and transparent input from stakeholders—local authorities, advocates, providers, public health, those in services, underrepresented populations. Stakeholder engagement is an important part of getting this right and we are committed to that.
What is the proposed timeline for the consolidation?
We have built a long runway and a capable team to implement any changes. From the time of the bill’s enactment in the 2021 General Session until the end of the current calendar year (2021), the Department of Health and the Department of Human Services will identify and conduct a review of all of the elements critical to a successful merger including structure, personnel, state and federal grants, contracts and services.
During the same timeframe, significant stakeholder outreach would be conducted by the leadership of the departments to address outstanding stakeholder concerns, ensuring the success of the new agency, and that the preferred template is adopted.
● By December 31, 2021, following consultation with the Governor’s Office, legislative committees of jurisdiction, and utilizing limited rule-making authority, the combined agency would adopt the best template for the newly merged agency.
● During the 2022 General Session, additional legislation would be passed to codify the rules and template of the newly formed agency. This would also give the legislature the opportunity to give additional legislative direction to the newly merged agency.
● By June 30, 2022, the newly merged agency would become legally and fully operational as the Utah Department of Health and Human Services.
How will the agencies plan for this consolidation while managing the COVID-19 pandemic response?
We are moving in a positive direction in our efforts to address the pandemic, and we look forward to the day when it is no longer our main concern. We recognize, however, that the needs of our underserved communities will not go away. Delivery of vital services and programs has not stopped, and we have the opportunity to address needs moving forward.
The departments and the Executive Office of the Governor are unified and committed to a successful consolidation of agencies and to ensuring there is no disruption in service for customers. We have competent leaders and staff to provide technical expertise and support. We recognize that it would be a heavy lift for leadership and staff during the pandemic, but are confident it is achievable with legislative support, resources and the right plan in place, including input from stakeholders and service recipients.
Why is legislation needed first?
We believe that having legislation at the front end gives department leadership clear direction, authority and priority to plan and return to the legislature to present the approach determined with stakeholders and the public. Having a clear mandate early on from the legislature and working together with the public and the Office of the Governor gives us confidence the process can be completed in the next year and a half.
It is critical to note that upon passage of a bill in the 2021 General Session, these agencies will not automatically be merged into one. Authorizing legislation is critical to get the process started and properly studied, and for obtaining stakeholder input.
Who will lead the new Department and what qualifications will they have?
All three agencies have strong leadership in place to create the plan for a consolidated agency. They will work together as a team to develop the new agency structure that would be adopted by the legislature. The cabinet lead and the head of the new agency, as well as their qualifications and areas of expertise, will be up to Governor Cox. Stakeholder input into agency leadership is welcome as we focus on planning and ensuring we continue to provide an excellent level of service.
Health and Human Services is combined at the federal level and in many other states. Will those models influence how we combine programs through this consolidation?
It makes sense for us to be aligned with our federal counterparts to allow agency-to-agency communication on a more streamlined basis. We have also looked at the approaches of several other states. We acknowledge that no system is perfect and we will incorporate lessons learned from other models as we move toward better coordinated services in the state. We will do what works for Utah and not repeat inefficiencies we see in other models.
Will jobs be cut as part of the consolidation?
The Executive Office of the Governor is not proposing a reduction in the number of state employees as part of the proposed consolidation of agencies. If the change is approved by the legislature, and after studying combined agency functions, any workforce reductions would be through attrition, and not through a reduction in force.
We will work with the Legislature to ensure that staff performing critical functions are retained and that there is neither a reduction in employees charged with these critical functions, nor a reduction in the quality of services offered to the residents of Utah.
How will the integration of behavioral health and physical health improve care for those with co-occuring conditions?
We have been working over the past several years to determine how best to coordinate and integrate physical and behavioral health care. Risk and protective factors are similar. Our ultimate goal is to provide a more complete approach to prevention efforts, direct services, and better care.
When a family or individual comes to an agency for services, the model should include a needs assessment from a family perspective and evaluation of their health care needs. There would be a full assessment of those needs in the consolidated agency model. Bringing resources together would help us address these factors in a comprehensive and cohesive way.
What parts of Medicaid will move to Workforce Services?
Utah is unique in that Workforce Services also handles eligibility for economic support. Things are working well in our state with eligibility linked to workforce programs. There is an opportunity to connect families to a single entity for economic support services.
The agency consolidation bill would move Medicaid eligibility components from the Department of Health to Workforce Services. These functions include Medicaid eligibility policy, Medicaid Eligibility and Quality Control (MEQC), and eligibility adjudications.
The components of Medicaid that would move to Workforce Services will not impact the current customer experience. The access point will be the same. Workforce Services will assume responsibility on policy development (in collaboration with the Department of Health and Human Services) and quality control (Workforce Services currently manages quality control for SNAP). The Department of Health (as part of the consolidated Department of Health and Human Services) will continue to manage oversight for Medicaid. There are still nuances that need to be sorted out. Alignment is important—we are working out what the final structure looks like.
How specifically will this impact contracted Medicaid-Medicare program providers?
No changes are intended to the functional Medicaid-Medicare program processes. Eligibility would continue to be managed by Workforce Services; the Department of Health (consolidated within the Department of Health and Human Services) would continue to manage medical requirements and policy for benefits.
Will there be any change to the Medicaid Inspector General?
The Office of the Governor is not proposing to collapse that independent office into this consolidation. We have asked the inspector general for direction on how to improve Medicaid audits and oversights, and other areas where there might be gaps.
Will the Medicaid changes impact individuals who are currently being helped?
People receiving services would not experience a disruption or delay in their services, or a change in eligibility. For the front-end user, it would be a seamless transition. However, we do expect improvement in internal communication and processes.
The Department of Health and Department of Human Services will continue to manage the services portion of Medicaid eligibility. As part of implementation planning, we will review impacts and solicit feedback on individual and family stability, efficient delivery of quality services, communities of color, and private providers and partnerships.
How will Medicaid waivers be managed?
Currently, some Medicaid waivers are managed by the Department of Health and some are managed by the Department of Human Services. Under the proposed restructure, Medicaid waiver management will be consolidated to maximize efficiency and eliminate complexities for providers and people receiving services. We will ensure no programs are left behind.
How will individualization, access and quality of services improve?
The primary reason for agency consolidation is to improve the quality of, and access to services. Artificial silos between mental and physical health, or individual and community health, impede prevention strategies and access to services, and are counter to our collective mission to treat the totality of needs of individuals, families and communities.
Traditionally, the Department of Human Services has addressed individual interventions, while the Department of Health has been more focused on community health. Agency consolidation presents an opportunity to combine our perspectives and coordinate our respective strengths by looking at common risk factors and social determinants of health around issues such as chronic disease, suicide, substance use disorders and elder care.
We will engage stakeholders at every stage of planning and keep service delivery at the forefront to ensure we understand community needs and can target resources effectively.
How do we see this change increasing access to services at the local level?
If state agencies are the lungs of health and human services, local agencies and provider networks are its capillaries. It is vital that we treat it as one system and strategize effective service consolidation and integration at all levels. A unified mission and message communicated at every level simplifies expectations and enhances accountability for our local partners on the front lines delivering services.
Do we expect changes to billing or how state and federal funding is distributed among providers?
Our intention is to minimize disruption for people receiving services as we undergo agency consolidation. The current claims payment system will remain the same. We will continue to have discussions with stakeholders to identify and address opportunities as we go forward.
How will the restructuring complement the state’s homelessness system?
Though this agency consolidation does not directly affect homelessness governance, it does create opportunities for synergies around economic, behavioral and health issues commonly occurring for people experiencing homelessness such as substance abuse, mental health and chronic disease. Managing these areas can positively impact upstream issues like housing.
These agencies are often the first stop for highest cost and greatest need individuals. How will merging agencies impact these populations?
Siloed services are currently a significant hurdle for high-needs individuals and create potential for people to “fall through the cracks.” Consolidation would help agencies keep track of these individuals and ensure they are receiving appropriate services.
Three prevelancies in high-needs populations include behavioral health, physical health and financial supports. By consolidating social services, we would align divisions that address these needs, such as mental and physical health providers and the Medicaid program to best serve the whole needs of an individual.
There is always room for improvement when it comes to serving individuals and families with acute and complex needs. Those who are served will be at the forefront of our planning and asked for feedback during this process.
How will duplication of services be resolved through agency consolidation?
There are a number of overlapping areas of focus among the Department of Health, Department of Human Services and Medicaid where services could be combined and redundancies reduced. Some of these areas include suicide prevention, substance use prevention, domestic violence, and services for aging adults. Currently, some individuals and families interact with multiple agencies and case managers, which complicates service delivery. A consolidation of agencies and alignment of Medicaid eligibility would provide streamlined solutions.
Merging these functions would not only be an opportunity to eliminate redundancy, it would combine practice approaches and make services in these areas more robust. Each agency’s approach has its own unique strengths; bringing them into alignment will help us be more effective.
Is there a possibility of costs increasing through the consolidation?
We know we have to be responsible for how funds are used. We are awaiting a report from the legislative fiscal analyst after the bill is drafted. Agencies will participate in that process.
A consolidation of agencies could provide the opportunity to be more efficient with state funds and, ultimately, we believe there would be favorable cost outcomes. The cost of the merger has been accounted for in the Governor’s budget.
How will the merger maximize taxpayer dollars and efficiency?
Currently, inefficiencies stem from overly complex bureaucratic processes and siloed services. Program alignment, interagency coordination and elimination of administrative redundancies would all maximize efficiency and efficacy. Savings created through efficiencies would be reinvested in improving and increasing access to services.
Have we projected cost savings and where the savings would be utilized?
Potential cost savings have yet to be quantified because we are at such an early stage in the process. We intend to work with legislative committees to ensure any savings are reinvested in the department and available as enhanced services for customers.
How will data or metrics be used in planning?
It is important to have a clear, unified vision of what success looks like and how to measure it so that we can work collectively and strategically toward our objectives. We are in the process of developing these metrics. Heath and Human Services are both disciplinary areas driven by evidence-based, data-driven research and practice models. We believe that consolidating agencies would reduce challenges created by service silos and enhance our ability to measure outcomes.
Combining agencies would remove barriers to data sharing among agencies and allow us to more accurately evaluate families’ needs and provide appropriate, accessible services. Currently, individuals and families are coming to Workforce Services for economic support, to the Department of Health for physical health services, and to the Department of Human
Services for social services and support. Although the same family may be accessing services from multiple agencies, it’s difficult to track and share data among them. Having the same mission, vision and management will help us improve services.
###